A nursing note is a medical or health record that is made by a nurse that shows accurate documentation of nursing assessments, changes in patient’s conditions, care provided, and related information to support the clinical team to deliver excellent care.
Keeping a detailed and accurate note is essential for having efficient communication between the medical staff and nurses. This serves as a proof of record between the medical staff and nurses to show the progress achieved in a patient and guide whoever takes off after the previous working staff of a day. Apart from record purposes, the legal team uses it or chart in case of any lawsuit or malpractice to show what was last noticed in the patient and what was the last action taken to treat him or her.
It would help a nurse recall the nature of the events and care provided and the doctors involved if she is called as a witness or sued.
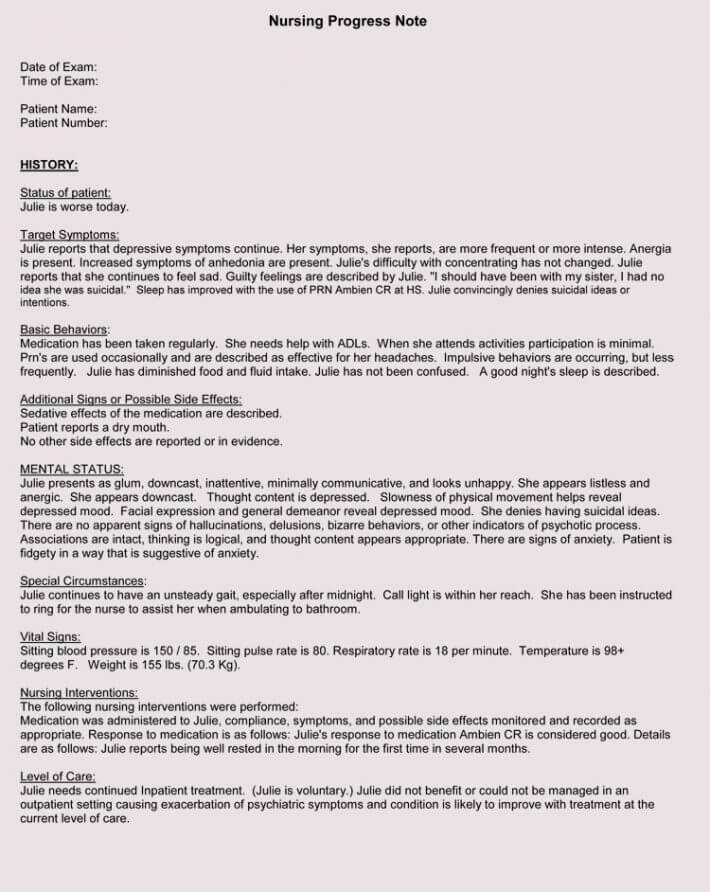
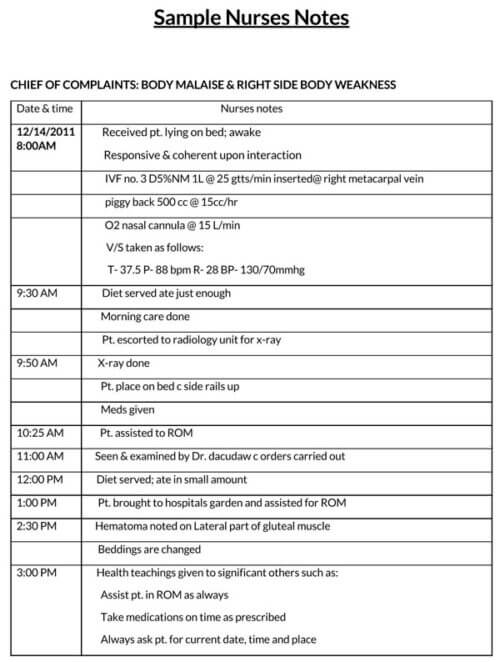
Note Templates


Things to Know When Writing It
When writing a note, the nurse should consider the next staff attending to the patient as they would be the one using it. They should also be thinking long-term as references to the note might be needed in the future. A complete summary of the patient’s condition, treatment administered, and improvements should be documented appropriately.
The listed should be stated correctly in the note:
- The Date and time
- The Nurse’s Name
- The Patient’s Name
- The Reason for Visiting
- The Patient’s Assessment
- Vital Signs or Symptoms
- The ordered Labs and Diagnostics
- Medical Intervention Evaluations
- The Instructions
- The Family Interaction
- Observations and Recommendations
For whom it is written?
When writing it, the aim is to communicate a patient’s medical treatment journey to the next medical staff, a lawyer, the state or even your superior. Write to provide very standard information as if to a state. This way, the note would be appealing to whoever is reading it.
These are kept with the hospital management as this would help the stakeholders for whom it is meant to have access to it quickly without issues.
When are Nursing notes written?
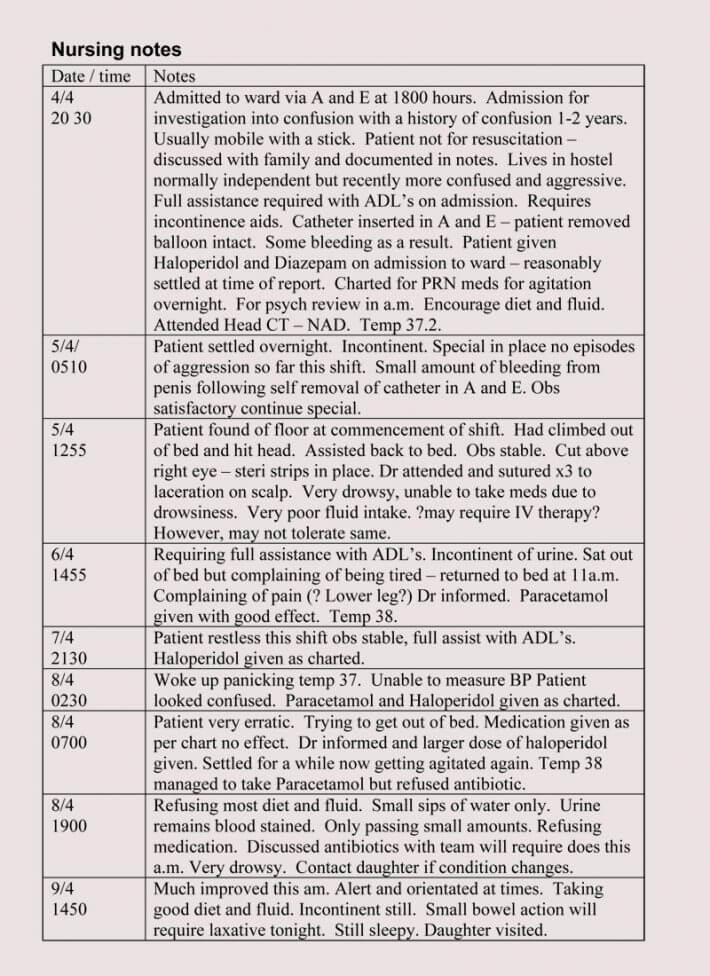
These can be made during patients’ visits. It can also be written quickly after leaving the patient’s corner when the details are still fresh.
Fill it out within 24 hours of supervising the patient’s care. It’s important for it to be ready for the next person who is going to be working the shift after you.
Nursing notes vs. charting
A nursing note is a part of charting. It shows the period when things are done or said. On the other hand, charting includes all the notes plus graphs. It is interpretative, while charting is objective.
Types
The main types include:
- Ongoing documentation notes: An ongoing documentation note sums up what action nurses take on patients regularly. It is routine documentation that helps the nurses keep tabs on the treatment and progress of patients throughout the whole course of their medical therapy. It is essential as it helps substantiate the nurse’s job and trend of treatment.
- Health notes: A health note is an important one that shows changes in a patient. It is usually used to document improvements and regressions or even side effects that treat effects in people. The nurse can use it to record even change in treatment, e.g. changes in injections or medications administered to the patient. Health notes can consist of discharge notes, admission notes, and fall notes.
- Incident notes: These are made by nurses in case of incidents. Incidents could be complicated with complex details. Thus, it is essential to pay close attention in writing the events or happenings as it unfolds.
These notes are more likely to be needed or reviewed during a lawsuit. Ensure to write them well, presentable, and engaging. - Behavior notes: The behavior note is 100 percent psycho-social and is related to incident ones. They mainly involve people making threats to other’s security. Under this type of note, nurses record notes on a patient’s behavior involving aggressive behavior, fights, and threats to others.
- Communication notes: As the name sounds, it is the documentation that makes other hospital staff know more about the patient. This note is mostly on simple but essential things like sending a fax. Its main aim is to reveal some vital information not readily known by other staff.
- Death note: Death note is another type of important nursing note. It is primarily direct. It would be extensive in the case of accidental death. Thus, it should involve any timestamps or details associated with the patient.
The nurse should note what happened and what didn’t happen, and why it didn’t happen.
Structuring the Notes
Nursing notes can be structured appropriately using the SBAR method; Situation, Background, Assessment, and Recommendations.
Situation
Start it with a straightforward summary. Write the first lines so people can know what it is attempting to address. Start it with the necessary elements so that readers can know the nature of the situation on notes.
Background
The background presents a summary of the origin of the patients’ condition and what treatments have been administered in the past. The background should carry enough information to enable the medical personnel to know the next line of action to take.
More so, write notes or sentences that leave no room for more questions or guessing. When writing an important one, consider asking another nurse to help so that everything would be effectively captured.
Assessment
Assessment section explains where to give an opinion using the scientific data gathered. The assessment should be on what happened, including the raw data found. The clinical evaluation after the assessment should be used to make recommendations.
After the clinical assessment, the next thing is to register the findings and list them out. Write out the relevant clinical results of the patient. Other staff might use it to take care of the patient later in the future.
When assessing, consider the following; Medications, Health history, Distress, Vital signs, Progress notes, Diagnosis, and Psycho-social.
Recommendations
As a nurse, the recommendation or actions would be based on the clinical assessment. This also involves documenting the remedies administered on the patient and improvements as a result of those remedies.
Good documentation can be challenging. It involves creating a note that can be engaging and can speak for itself. It should be accurate and leave no room for further issues or questions. Always re-read and edit them to create clear, compelling, and lasting content.
Standard Format
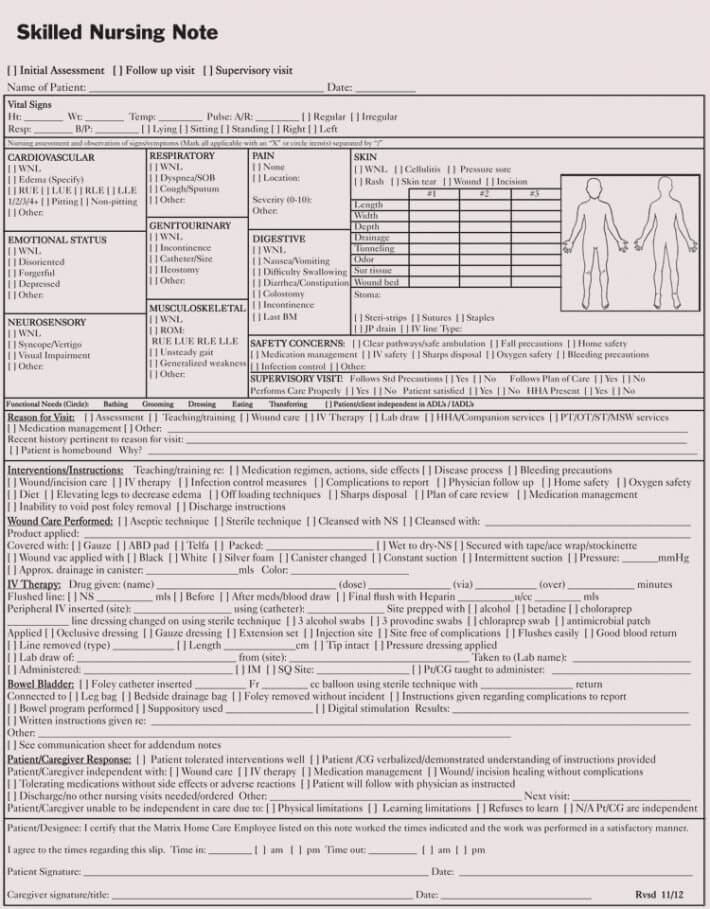
First thing that goes on the note is the patient’s information. This includes the patient’s name, arrival time, and departure time. Next is the patient’s vitals. This includes:
| Temperature: | Universal Precautions Followed: |
| Respiration: | Hand washing, gloves worn, sharps disposal, alcohol, gel/hand cleanser, other: |
| Apical Pulse: | Homebound Status: |
| Radial Pulse: | Coordination of care: RN, LVN, therapist: |
| Next is Physical Assessment: | HHA, MSW Discussion: |
| Respiratory: | Physician contact: N/A, Yes, Discussion: |
| Gastro Intestinal: | Discharge Planning: |
| Neurological information: | 5 Day Discharge notice given to patient/physician: |
| Ears/Eyes/Nose/Throat: | LVN/HHA Supervision: |
| Musculoskeletal: | Patient/caregiver satisfied with care: |
| Circulatory: | Change in ADL needs assessment: |
| Skin Conditions: | Care provided according to assignment: |
| Gu Status: | Employee courteous, respectful: |
| Under that is the Pain Assessment Notes: | Continue Frequency at: |
| Pain or No Pain: | Supervisory visit onsite: |
| Location, Duration: | Employee Name: |
| Intensity on a scale of 1-10: | LVN, HHA: |
| Under that goes current pain medications: | Instructed in: |
| Glucometer: control | Date: |
| Results: FSBS, RBS | Wound Care: |
| Under that is Skilled Nursing Care Performed: | Signs/symptoms of infection: |
| Additional clinical findings: | Teachings of wound care: |
| Progress Toward Goals on POC: | Dressing Change: |
| New identified problems/goals: | Additional Comments: |
Always Workable Things
There are things workable, and those that are termed normal and abnormal assessments to know to have a great note:
On normal assessments
These are clinical assessments that are workable. Some of them include:
- no s/s of pain, distress, or breath shortness.
- The patient revealing his needs
- The patient couldn’t make decisions.
On abnormal assessments
Nurses should properly document ailments or events covered or treated that involved abnormal assessments; For example, The patient involved in a witnessed fall.
- The patient found on the ground
- The patient at considerable risk for fall
- The patient who doesn’t follow instructions
- The patients who run away without permission
Not-to-Include Things
The things not needed to include:
- Patient’s personal information: Do not include personal information concerning the patients’ family members and friends. No information that is too personal should be included.
- Dialogues with providers: Do not input the dialogues about patients between the providers. The nurse should only state what she has told some physicians.
- ISMP Abbreviation list: Do not include anything from the ISMP Abbreviation lists. The abbreviations from this list can be misinterpreted and could even create some medication errors.
- Personal Opinion: Instead of putting personal opinion, recommend the systems or staff deemed necessary.
- Negativity about the staff: Don’t write negativity about other staff. It could be seen as defamatory. Reporting staff problems can be reported in a way that won’t create any issue in the hospital.
EXAMPLE
“The senior doctor didn’t show concern at all to the patient” can be reported as; “the senior doctor wasn’t aware of the patient’s grave issue.”
Key Points to Follow
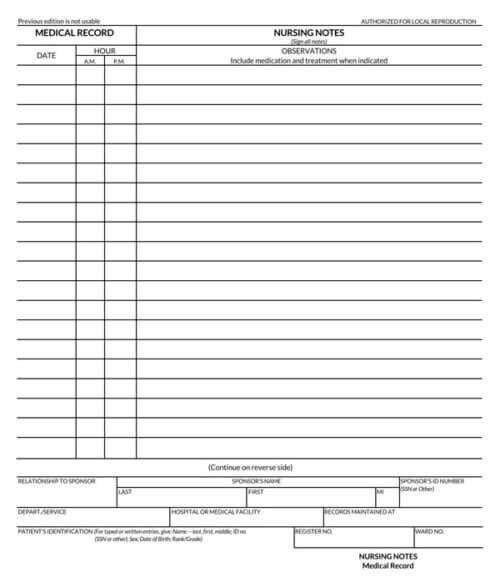
Always Use A Consistent Format: Start the record with the patient’s ID information. Remember each entry should include your full name, the date, and the time of the report as well:
- Write Neatly: Please write the notes clearly and neatly. If no one can even read your notes then they are basically useless. Take your time when writing down the information.
- Keep Your Notes Simple: Don’t write down irrelevant information that has nothing to do with the patient’s health. Nursing notes are supposed to be designed to be read quickly. That way the next shift will be caught up on the patient. Be clear and concise. Only add the key and necessary terms and try to keep it short.
- Always Write Down All Communication: Write down everything important about the patient’s health. Every single discussion you had with the families, doctors, and other medical professionals needs to be documented. Also, you need to document the names of the people you had these discussions with.
- Please Don’t Use Abbreviations: Write everything down fully. Using abbreviations can mean different things in different places.
- You Should Write As You Go: As a nurse, you’re supposed to complete all of your notes as soon as possible. So with that in mind, you should not leave it until the end of your shift. Just write as you go. That way all the information from your notes will be fresh in your mind.
- State the facts: A nurse should only write or chart what she hears, observes, and does.
- Find a mentor: Another tip is to search for a veteran or experienced nurse to offer guidance and constructive feedback.
- Check out other nurses’ notes: Check out how other nurses, mainly veterans write their nursing notes. It will guide and influence a good note.
- Have Summary mindset: Good summaries are helpful to anyone involved with patients. There should be a summary readily available in every patient’s charts in each hospital visit.
- Keep note of the responses: Write how the patient replied to the treatment. Note if they adhered to the doctor’s advice or nurse’s guidelines.
- Don’t Speculate: Do not assume or speculate. Always write the patient’s feelings, and mainly write what the patient says.
- Note the patient’s observations: Note the necessary observations with the patient—some pertinent patient observations like swelling, extreme pains, and the color pink need to be noted.
Conclusion
The reason for writing it is quite simple. It helps the nurse have a breadcrumb trail on how the patient was treated and improvements or regressions encountered in the process. Think about the type of information others (other nurses) need to know and events that happened. The note should be clear and concise to make enough sense to its reader at one glance.